You Are Not Your MRI
Magnetic Resonance Imaging (MRI) is “a noninvasive medical imaging technique that uses radio waves and a strong magnet to create detailed images of the inside of the body,” according to AI after a quick Google Search. It is typically classified as the “gold standard” to assess various soft tissue conditions throughout the body.
So, let’s say you developed a sore shoulder after picking up pickleball last week. You see your doctor, who orders an x-ray and refers you to a physical therapist. The radiograph (x-ray) was negative and you may wonder, “do I need an MRI?” Wouldn’t an MRI help determine what the problem is? The answers to those questions are a bit more complicated and murky, and this post will hopefully give you an idea as to why.
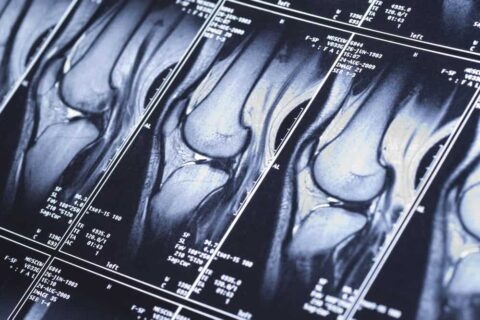
The first thing to point out is pretty intuitive and doesn’t need a fancy citation: MRI is a static picture of your body in what we call “anatomical position.” MRI does not provide any insight as to how that muscle, joint, ligament, etc, functions throughout your range of motion or how it responds to loads that you need to put through it. It is also difficult to accurately determine the acuity of any abnormality found on MRI. A retrospective study in 2021 in the International Journal of Spine Surgery tasked 2 trained raters to attempt to determine the acuity of the symptoms of 89 patients via their MRI images only and found that there was no inter-rater reliability between patients with acute and chronic low back pain and their MRI characteristics.
Inter-rater and inter-machine reliability was also brought into question in a 2016 article in which a single 63 year old woman with low back pain presented to 10 different MRI centers over a 3 week period. 49 distinct findings were found by the 10 radiologists with 33% of those findings found on only one report and only one finding found across 9 out of 10. Nothing was found across all 10 reports. This suggests that 32-55% of MRI findings in this study had the potential to be false-positives or errors in interpretation.
To be fair, these are only two studies with two distinct suggestions. So let’s pretend that what the report suggests is true. How likely is that finding the cause for the symptoms that you are experiencing?
There is an extensive list of studies that involve taking asymptomatic volunteers and obtaining MRI of their shoulder, neck, back, knee, etc to try to assess the incidence of common MRI findings. The numbers may surprise you!
Low Back:
- A systematic review in 2015 of studies covering 3110 asymptomatic individuals found that prevalence of non-painful disc degeneration was 37% in 20-year-olds and jumped with each decade to 96% in 80-year-olds, disc bulge prevalence was 30% to 84% for the same decades.
- This study concludes: “Imaging findings of spine degeneration are present in high proportions of asymptomatic individuals, increasing with age. Many imaging-based degenerative features are likely part of normal aging and unassociated with pain.”
Shoulder:
- A 1999 study of 411 asymptomatic volunteers found rotator cuff tears in 23% of volunteers with prevalence associated with age range moving from 13% of 50-year-olds to 51% of 80-year-olds increasing in prevalence with each decade
- In a study of 588 patients with pain in one shoulder, 177 had bilateral rotator cuff tears despite only one shoulder being painful.
Neck:
- A 1998 study of 497 asymptomatic subjects found non-painful discogenic pathology in 15% of 20-year-olds and as high as 89% of folks over 60.
Knee:
- A study of 85 asymptomatic folks over 40 years old found that 50% displayed presence of osteoarthritis.
- A 2020 study of both knees of 115 asymptomatic sedentary adults, with the median age of 44 years old, found that 97% of knees showed at least 1 abnormality on MRI.
- Finally, a systematic review in 2020 of 63 studies including 5397 knees across 4751 asymptomatic adults found that prevalence of osteoarthritis ranged from 4-14% in folks under 40 and 19-43% in folks over 40.

So what do all these numbers mean and why might they be important to you? Our hope is to normalize some of the words you may hear from your physician, such as “osteoarthritis” or “rotator cuff tear.” We encourage an understanding that without a significant mechanism of injury, all of these conditions can be present in happy, asymptomatic folks across the world! While finding the “smoking gun” is incredibly alluring, the reality is that most folks come to us because of the rule of too’s: too much, too soon, for too long. With some skilled intervention, a little bit of time, and some work on your part, participating in Physical Therapy can get you back to all of the activities that you were doing before that shoulder started giving you problems. You will be back hitting those overhead smashes on the pickleball court in no time!
TL:DR – MRI is a static picture in anatomical position and does not account for time, acuity, or function. With the help of a Physical Therapist to break down the movements that are uncomfortable, improve your tolerance to them, and build them back together, you can get back to all of your preferred activities without worrying about what that image says!
If you or a loved one are dealing with a nagging sports injury, pain, or are in need of post-operative rehab, we can help! With convenient locations in Stoughton & Foxborough, Elite has a team of highly trained Physical Therapists who will work with you to decrease your pain, improve your strength, mobility and function, and get you back to enjoying your favorite activities and an active lifestyle. To schedule an appointment with one of our PTs, visit HERE for more details!
Author: Andrew Guay, PT, DPT, OCS
Citations:
- Divi, S. N., Goyal, D. K. C., Makanji, H. S., Kepler, C. K., Anderson, D. G., Warner, E. D., Galetta, M. S., Mujica, V. E., Houlihan, N. V., Kaye, I. D., Kurd, M. F., Woods, B. I., Radcliff, K. E., Rihn, J. A., Hilibrand, A. S., Vaccaro, A. R., & Schroeder, G. D. (2021, June 1). CAN imaging characteristics on magnetic resonance imaging predict the acuity of a lumbar disc herniation?. International Journal of Spine Surgery. https://www.ijssurgery.com/content/15/3/458.abstract
- Variability in diagnostic error rates of 10 MRI centers performing lumbar spine MRI examinations on the same patient within a 3-week period – the spine journal. (n.d.). https://www.thespinejournalonline.com/article/S1529-9430(16)31093-2/fulltext
- Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., Halabi, S., Turner, J. A., Avins, A. L., James, K., Wald, J. T., Kallmes, D. F., & Jarvik, J. G. (2015, April 1). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American Journal of Neuroradiology. https://www.ajnr.org/content/36/4/811.short
- Tempelhof, S., Rupp, S., & Seil, R. (1999). Age related prevalence of rotator cuff tears in asymptomatic shoulders. Journal of Shoulder & Elbow Surgery, 8(4), 296-299.
- Yamaguchi, K., Ditsios, K., Middleton, W., Hildebolt, C., Galatz, L., & Teefey, S. (2006). The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. The Journal of Bone & Joint Surgery, 88, 1699-1704.
- Matsumoto, M., Fujimura, Y., Suzuki, N., Nishi, Y., Nakamura, M., Yabe, Y., & Shiga, H. (1998). MRI of cervical intervertebral discs in asymptomatic subjects. The Journal of Bone & Joint Surgery, 80(1), 19-24.
- Fukuta, S., Kuge, A, & Korai, F. (2009). Clinical significance of meniscal abnormalities on magnetic resonance imaging in an older population. The Knee, 16, 187-190.
- Horga, L. M., Hirschmann, A. C., Henckel, J., Fotiadou, A., Laura, A. D., Torlasco, C., D’Silva, A., Sharma, S., Moon, J. C., & Hart, A. J. (2020, February 14). Prevalence of abnormal findings in 230 knees of asymptomatic adults using 3.0 t MRI – skeletal radiology. SpringerLink. https://link.springer.com/article/10.1007/s00256-020-03394-z
- Culvenor, A. G., Øiestad, B. E., Hart, H. F., Stefanik, J. J., Guermazi, A., & Crossley, K. M. (2019, October 1). Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: A systematic review and meta-analysis. British Journal of Sports Medicine. https://bjsm.bmj.com/content/53/20/1268
